Prosthetic process for lower extremity amputees
A human body part may be missing due to trauma, disease, or conditions present at birth. A prosthetic or prosthesis is an artificial body part used to replace a missing body part. “Prosthetics” describes the art of making and fitting a prosthesis.
Below is information regarding the prosthetic process, with a brief description of stump shrinkers, test sockets and prosthetic legs, and insurance considerations. Also, information about wound care since many amputations are related to foot wounds.
We specialize in adults with lower extremity amputation, above-knee (AK), below-knee (BK), ankle, or foot.
For certain foot wounds, a custom orthotic wound care device may be prescribed by your doctor to off-load the pressure of weight-bearing on the foot, and hopefully prevent amputation.
For new amputees, see our handout: Initial Prosthetic Process: An Overview for New Amputees
Para nuevos amputados, consulte nuestro folleto: Proceso protésico inicial: Descripción general para nuevos amputados
1. Stump shrinker
The first prosthetic component is compression hose for the residual limb following amputation; not all patients require a stump shrinker.
- made to measure from compressive knitted material
- helps to control swelling of the residual limb; shape the stump; control swelling when prosthesis is off
- usually applied after surgical staples are removed; may be applied during the rehabilitation period, before the incision is completely healed, or if requested by the physician

2. Test socket
In order to make a preparatory prosthetic leg, a test socket is created.
- the residual limb is cast to make a mold for the test socket
- the socket is clear in order to see boney prominences or potential pressure points
- the socket is used to make the final socket for the preparatory prostheses or training leg

3. Preparatory leg
The first prosthesis is the preparatory leg, which includes a socket, pipe, and foot. It is used as a training tool for gait training and physical therapy; to learn how to ambulate with the prosthesis; and to achieve the highest K-Level possible.
Usually, certain supplies are authorized each year, depending on the insurance provider. Supplies may include: 2 stump shrinkers; 6 multi-ply volume socks; 6 single-ply volume socks; 2 gel liners with pins.
As a patient increases their functional ability and adapts to the prosthesis, we constantly assess their gait and comfort level, and make adjustments and modifications in preparation for fabricating the definitive.
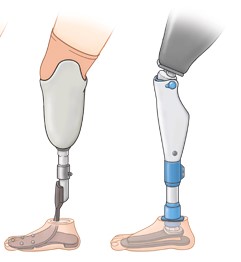
4. Definitive leg
The final prosthesis is the definitive. Patients should be completely satisfied with their mobility before having the definitive made.
Each individual is different, and it may many weeks or months to achieve their best mobility. When a patient has achieved their highest K-Level, and are confident in their prosthesis and its components, we request insurance authorization for the definitive.
Usually, patients may receive 2 gel liners each year, however supplies must be authorized by the insurance provider. Insurance usually authorizes a new definitive prostheses every 5 years, unless an earlier replacement is medically necessary (for example due to change in health, weight, ability). In the photo, our patient added a step-counter.

Considerations for insurance and benefits
Verify your insurance coverage.
Before starting the prosthetic process, it is important to verify your insurance coverage in order to understand your benefits, avoid unforeseen expenses, and be aware of possible out-of-pocket expenses.
This process can be time-consuming and confusing, so we can provide assistance to our patients with insurance verification and authorization.
We will work with you, your health care providers and your insurance, in order to achieve your highest activity level, and until you are satisfied with your mobility.
Patients have a right to two prostheses: (1) Preparatory leg, and (2) Definitive leg.
Protect your benefits.
Until you receive a prosthesis that meets your needs, don’t allow any company to file claims on your benefits. For example, do not sign for anything until you have a working product and are satisfied.
Know your rights.
You have the right to chooses your healthcare provider, and to change providers if your needs are not being met. Use available resources to become familiar with other rights to which you may be entitled (legal, federal, workplace, etc.).
You are the only one who knows what you need, so you must advocate for yourself. Explain your needs and any concerns you have to your prosthetist. At times when you don’t have energy to advocate for yourself, bring a family member or friend help.
K-Level
What is K-Level?
You will hear the term “K-Level.” Your K-Level is your mobility level, which will determine your eligibility for certain prosthetics and components.
K-Level refers to a classification system used by Medicare and insurance companies to indicate a patient’s function and rehabilitation potential. “K” is an arbitrary letter assigned to this system by the Health Care Financing Administration.
The K-Level system is a rating from 0 through 4. K-Level 0 patients are not physically capable to be considered for prostheses. Higher K-Levels are eligible for more high-tech, expensive prosthetic components, such as feet or knees.
K-Level 1-4 indicate a person’s potential to use a prosthetic device under these guidelines: if they have a device that works well for them; and if they have completed rehabilitation in order to use the device properly.
- K-Level 1 – household ambulator. Ability or potential to use prosthesis for transfers or ambulation on level surfaces at a fixed cadence.
- K-Level 2 – community ambulator. Ability or potential to transverse low-level barriers
(curbs, stairs, uneven surfaces). - K-Level 3 – high-level, high-activity community ambulator. Ability or potential to transverse most barriers at variable cadence.
- K-Level 4 – high-impact, high-energy levels such as children, athletes. Ability or potential for ambulation that exceeds normal skills.
Wound Care
Wounds can lead to amputations. For certain foot wounds, it may help to off-load the pressure of the weight-bearing on the foot, and hopefully prevent amputation. A custom orthotic wound care device may be prescribed by your doctor to off-load the foot wound.
Considerations for wound care
Wounds are very common when a patient has peripheral artery disease or diabetes; these diseases often cause loss of nerves and pain sensation, and the absence of pain can cause wounds to go untreated.
Over 5 million patients with peripheral artery disease also have diabetes, and each year nearly 100,000 have a leg amputation, over half of which are due to these diseases.1
Management of wounds to help avoid amputation includes routine comprehensive checkups and preventive care by your doctor, and may include:
- regular assessment of the color, texture, temperature, and nerve function of the extremities
- blood tests and medications, such as insulin to help control blood sugar
- referral as needed for comprehensive care involving vascular surgeons, specialized podiatrists, and wound managers
Interventions to improve blood flow may include:
- ankle brachial index (ABI) to measure blood flow in limbs;
- ultrasound imaging to determine artery narrowing;
- endovascular interventions such as angioplasty (using balloons, stents), atherectomy (removal of intra-arterial plaque), or bypass surgery.
- Barnes JA, Eid MA, Creager MA, Goodney PP. Epidemiology and risk of amputation in patients with diabetes mellitus and peripheral artery disease. Arteriosclerosis, Thrombosis, and Vascular Biology. 25Jun2020;40:1808–1817.
Resources
Exercises for the Lower Extremity Amputee
Pain and Phantom Limbs. War Amps 2013 published by The War Amps (Canada) with permission.
